

7 Proven Ways Credentialing Reduces Medical Malpractice Risk
Credentialing and medical malpractice risk are directly linked—learn how strong credentialing practices can protect providers and reduce liability.
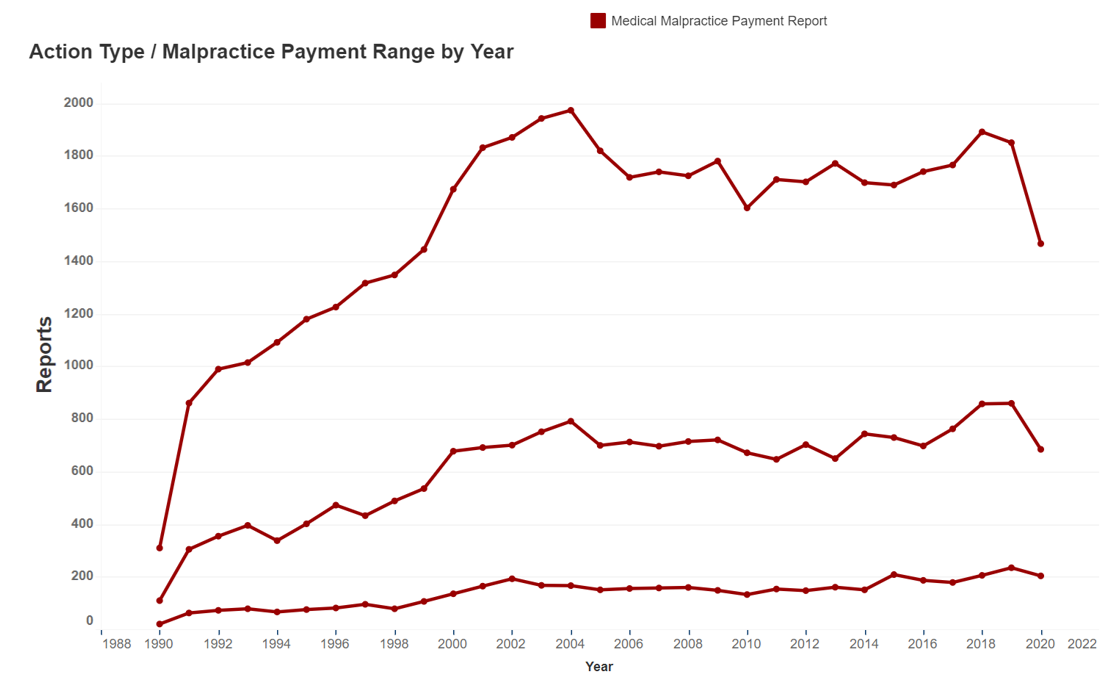
Per the NPDB, medical malpractice payment reports >$500,000
have risen over 544% from 1990 to 2020. This large increase demonstrates a complex risk environment. We can help.
The realm of medical malpractice is increasingly intricate and fraught with risk, as exemplified by the NPDB (National Practitioner Data Bank) data revealing a remarkable 544% surge in medical malpractice payment reports exceeding $500,000 from 1990 to 2020. In 2021, a noteworthy 51% of physicians faced medical malpractice lawsuits. These statistics underscore the imperative need for a comprehensive understanding of the intricate medical malpractice landscape to ensure adequate protection.
Fifth Avenue Agency proudly stands as an independent, specialized medical malpractice insurance agency. Selecting the right medical malpractice carrier entails a meticulous assessment of various financial aspects and crucial inquiries. Whether you are a healthcare provider, nurse, or part of a medical group, we collaborate with a diverse spectrum of healthcare professionals nationwide. Our status as an independent agency empowers us to prioritize the unique requirements of our providers above any specific carrier’s dictates.
Data sourced from the National Practitioner Data Base (NPDB) underscores a substantial 544% surge in medical malpractice payment reports exceeding $500,000 over the past two decades. The NPDB chart delineates this rise in medical malpractice payment reports from 1990 to 2020, categorized into three payment brackets:
The aggregate increase from 1990 to 2020 in the number of these medical malpractice payment reports is up over 544%. This remarkable increase underscores the complexity of the medical malpractice risk landscape, warranting careful consideration and preparedness.
Within the Fifth Avenue Healthcare Services family, Fifth Avenue Agency operates in close collaboration with our esteemed sister company, Primoris Credentialing Network. Primoris is a significant player in the healthcare industry, holding the distinction of being the largest Independent Practice Association (IPA) in the Midwest. This accolade is a testament to Primoris' extensive reach and influence, as it boasts an impressive network comprising more than 54 health plans and options. This substantial network not only reinforces our commitment to comprehensive healthcare solutions but also bolsters our ability to offer an array of choices and opportunities to our valued clients.
In addition to our partnership with Primoris, we are proud to be affiliated with 5ACVO, another vital member of our sister company network. 5ACVO is renowned for its exceptional expertise in the field of credentialing. Through innovative methods and meticulous attention to detail, 5ACVO has achieved remarkable results, including a striking 69% reduction in credentialing costs compared to traditional approaches. This translates into substantial financial savings for healthcare providers under our purview.
Our relentless pursuit of innovative solutions thrives on close collaboration with our sister companies. One remarkable innovation in our portfolio is the development of a proprietary data file that stands out as a game-changer in the realm of medical malpractice insurance.
This unique data file is meticulously crafted to provide our medical malpractice underwriters with a wealth of uncommon, robust data. It encompasses a wide range of critical insights, from historical claims data to emerging industry trends and risk assessment metrics. This comprehensive data resource empowers our underwriters to make more informed decisions and assessments.
The potential benefits of this proprietary data file are manifold. Firstly, it has the capacity to contribute to lower premium costs for healthcare providers, as it enables us to better tailor insurance coverage to their specific needs and risk profiles. Additionally, it serves as a powerful tool in reducing the administrative workload requirements for our providers, streamlining the application and underwriting process.
Our collaboration with sister companies forms the cornerstone of our value proposition, setting us apart in the healthcare industry.
By leveraging the collective strength of our sister companies, we gain access to an unparalleled reservoir of industry expertise, boasting over 385 years of cumulative experience within the healthcare sector. This wealth of knowledge equips us with a deep understanding of the nuances and intricacies of the industry, enabling us to provide unparalleled solutions and insights to our clients.
Furthermore, our commitment to innovation extends to continuous investments in proprietary technology advancements. As a family medical group, we prioritize staying at the forefront of technological innovation. These investments are geared towards enhancing efficiency, streamlining processes, and ultimately delivering greater value to our clients. Our dedication to embracing cutting-edge technology ensures that we remain at the forefront of healthcare industry advancements, providing our clients with the most effective and forward-thinking solutions available.
A thorough and effective medical malpractice insurance recommendation hinges on a comprehensive grasp of your unique medical liability profile.
To achieve this understanding, we undertake a meticulous analysis of your specific medical malpractice requirements. This in-depth examination enables us to tailor our approach precisely to your needs.
Following the analysis, we work closely with our affiliated sister companies, drawing upon their specialized expertise and resources to craft a custom-tailored solution that aligns seamlessly with your objectives.
Should you choose to proceed with our proposal, rest assured that we are committed to swift and efficient implementation, ensuring that your medical malpractice insurance needs are met promptly and effectively. Your satisfaction and peace of mind remain our top priorities throughout the entire process.
Contact us for an initial discussion or to setup a time to review your medical liability needs.
We will leverage any potential opportunity for cost and risk reduction through our unique IPA and CVO partnerships.
During the proposal stage, we provide you a custom solution based on your needs.
We will implement your chosen medical liability coverage. Our goal is to help reduce costs and help mitigate your medical liability.

Among our esteemed sister companies, Primoris Credentialing Network holds a prominent position as one of the largest Independent Practice Associations (IPAs) in the United States.
Since its inception in 2010, Primoris has diligently served thousands of healthcare providers, drawing upon an impressive collective industry experience that exceeds 385 years. This extensive knowledge base positions Primoris as a trusted partner in the healthcare industry.
Primoris offers a comprehensive range of services, including both delegated and non-delegated health plan enrollment, serving members with access to over 54 health plan and network options. What sets Primoris apart is its commitment to streamlined credentialing management, facilitated through an intuitive and user-friendly credentialing web portal.
Through our collaborative network of sister companies, we gain access to robust underwriting data, a valuable resource that can potentially lead to reduced premium costs for our clients. To learn more about the exceptional services and expertise offered by Primoris Credentialing Network, we invite you to visit Primoris’ website for additional information.
Our Fifth Avenue sister companies provide access to additional expertise.
Fifth Avenue Agency engages in collaborative partnerships with our sister companies, namely Fifth Avenue Healthcare Services, which encompasses Primoris Credentialing Network and 5ACVO.
This collaborative effort brings together a cumulative experience of over 400 years in the healthcare industry, making this wealth of expertise accessible to both our organization and our valued client partners.

One of our esteemed sister companies within the Fifth Avenue Healthcare Services network is 5ACVO, a subsidiary that operates under the broader expertise and support of Fifth Avenue Healthcare Services. Within the realm of healthcare credentialing, 5ACVO has achieved remarkable success by simplifying what was once a laborious and intricate process. Through meticulous refinement and innovative thinking, they have managed to streamline the traditional 52-step credentialing procedure into a remarkably efficient and user-friendly 6-step process.
Moreover, the advantages of partnering with a Credentialing Verification Organization (CVO) like 5ACVO extend beyond the reduction of credentialing steps. By leveraging their specialized expertise, there are more than 20 distinct strategies available for cost reduction, which can significantly impact the financial aspects of healthcare operations.
We invite you to explore our comprehensive resources and insights available on our website at 5ACVO.com.
We design medical malpractice solutions for the complex needs of the healthcare industry.
Our clientele spans a wide spectrum, encompassing solo practitioners as well as prominent hospitals. Whether an individual nurse practitioner requires personalized coverage or a healthcare system seeks comprehensive group medical malpractice insurance, our expertise is at their disposal.
Fifth Avenue Agency operates as a proud member of the Fifth Avenue Healthcare Services family. Within this collaborative network of sister companies, we synergize our efforts to expedite revenue generation and effectively manage medical liability for our clients.
Explore our award-winning, comprehensive medical malpractice and credentialing blog, which provides continuous updates and insights into the ever-evolving healthcare industry and medical malpractice trends. Our blog covers a wide range of topics, including impacts on future medical malpractice rates, credentialing, delegated credentialing, provider or payer enrollment, medical professional liability (MPLI), and medical malpractice.
Within our industry blog, you’ll find valuable and educational content, such as guides on the advantages of utilizing PECOS, the latest developments in Medicare, key takeaways from MPLI, and updates related to COVID-19. Additionally, we share news and information from health plans, strategic partners, and payors, ensuring you stay well-informed about the latest trends and advancements in the healthcare landscape.


Credentialing and medical malpractice risk are directly linked—learn how strong credentialing practices can protect providers and reduce liability.


Start 2025 prepared! Discover how to strengthen your medical malpractice coverage with emerging trends, risk management, and proactive policy updates.


Explore strategies for healthcare providers to protect against medical malpractice verdicts with tips on risk management, insurance, and high standards of care.
Join the ranks of thousands of healthcare providers, including doctors, surgeons, medical practices, rural hospitals, healthcare systems, and large medical groups who have entrusted Fifth Avenue with their medical malpractice insurance requirements.