Some people work hard to achieve simplicity. Others make simplicity work for them. 5ACVO has worked diligently to create this simpler credentialing process.
The Importance of Credentialing
Credentialing is a necessity for every healthcare provider. It is of the utmost importance for patients to know their providers are fully qualified to practice medicine and that it is safe to share sensitive information with those people.
Credentialing can eliminate providers who are deemed unfit to administer treatment to patients. This can help decrease patient injuries and deaths. Credentialing can also help medical practices and organizations minimize their chances of facing medical malpractice lawsuits. Litigation can ruin providers and their organizations, destroying their reputations and assets.
Some medical organizations perform the intricate procedure in-office using their staff workers. While some people might have adequate training to complete the job, others might not. Their lack of proficiency in medical credentialing can result in mistakes that hinder onboarding new providers. Any delays can also impede any revenue the office can receive once they start billing. Medical offices can lose money and sink further into the red.
Simpler credentialing with 5ACVO
Credentialing with the team at 5ACVO can produce the following results:
- Lower the paperwork burden on medical providers by 88%.
- Cut costs by 69%.
- Complete the process 5-7 days faster than in-house credentialing.
5ACVO is a credentialing verification organization with clients in 20+ states. They concentrate on providing a simpler credentialing process, reducing overhead costs, increasing access to expertise, and speeding up the entire credentialing process.
5ACVO Reduces 52 Conventional Credentialing Steps Down To 6 Simple Steps
Although conventional credentialing is complex, 5ACVO has simplified the arduous process and created a simpler credentialing process. They have reduced the necessary steps to obtain a complete file from 52 conventional credentialing steps down to 6 simple steps.
52 conventional credentialing steps include:
- Sending out, tracking, and receiving the provider application packet.
- Obtaining the provider’s release.
- Obtaining the privilege forms.
- Reviewing the disclosure’s questions and answers.
- Reviewing the explanations of time gaps and claims history.
- Reviewing medical malpractice claims history.
- Obtaining applicable certificate copies of Board, ECFMG, Medical School, Internship, Residency, Fellowship, and two years CME.
- Obtaining copies of government-issued photo ID, Malpractice, DEA, and CDS.
- Obtaining CPR, ACLS, and PALS certificate copies.
- Obtaining TB, MMR, varicella, and flu vaccination records.
- Attesting any conflict of interest.
- Collecting a provider release and ordering a criminal background check.
- Obtaining an Allied Health Professional’s Supervising Physician’s Statement.
- Verifying Board certification.
- Reviewing and confirming AMA and AOA Profile.
- Verifying medical school internship, residency, fellowship, and affiliations.
- Confirming state medical licensure.
- Obtaining professional peer references.
- Gathering current medical malpractice claims history.
- Researching primary and out-of-state licenses for disciplinary actions.
- Verifying DEA certification.
- Verifying CDS certification (if applicable).
- Obtaining a copy of the provider’s current certificate of insurance.
- Verifying any Medicare and Medicaid sanctions (OIG) and exclusions (SAM).
- Performing an extensive 10-year criminal background check.
- Running a National Practitioner Data Bank query.
- And more.
5ACVO has taken all these time-consuming steps and pared them down to 6 simple steps creating a simpler credentialing process (three steps for initial primary source verification and three steps for reappointment credentialing).
These six simple steps are required for initial primary source verification and re-credentialing:
- Provide 5ACVO with a signed release.
- Evaluate the completed file from 5ACVO.
- Present the evaluation to the necessary board for a decision.
- Recredentialing (every 2-3 years): Provide a signed provider release.
- Recredentialing (every 2-3 years): Evaluate the completed credentialing file provided by 5ACVO.
- Recredentialing (every 2-3 years): Present evaluation to your committee or board for final decision.
5ACVO has pioneered simpler credentialing. Simplifying the credentialing process to six steps yields providers with lower costs and less work. Leveraging this service can be an effective business strategy. However, simple credentialing does not end here.
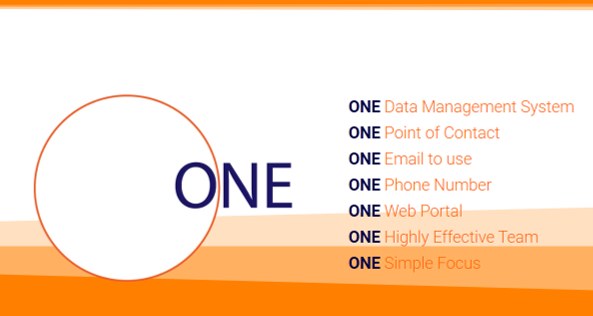
Simpler Credentialing With ONE Simple Focus
Simplifying the credentialing process has taken years of investing in the best technology and the finest people. 5ACVO’s primary focus is to practice administrative simplicity. They aim to provide easier credentialing by streamlining the process. While they have curtailed the work that goes into verifying physicians, they have also maximized efficiency across the board.
To help simplify the credentialing process, our providers have ONE point of contact.
- ONE Point of Contact: 5ACVO gives its users ONE point of contact for all your credentialing and primary source verification needs. This point of contact is a member of 5ACVO’s highly experienced team. Users only have to remember ONE email address and ONE phone number to get credentialing help, ONE user id login to the credentialing portal.
- ONE Highly Effective Team: 5ACVO is backed by 385+ years of combined industry experience. This knowledgeable team has the expertise to develop and perfect the credentialing process. By simplifying the process, 5ACVO can help providers and administrators with the effectiveness demanded in today’s challenging world. Verifying providers faster means billing can begin as soon as possible.
Technology and people are the core elements of 5ACVO. Without them, 5ACVO would have never reached administrative simplicity, which means that the industry might still be dealing with a long and expensive credentialing undertaking for every provider that needed validating.
Simpler Credentialing With Administrative Simplicity
Through determination and applied mastery, 5ACVO provides administrative simplicity for users:
- ONE point of contact,
- ONE email
- ONE phone number
- ONE experienced team
- ONE simple solution
Simpler credentialing must include administrative simplicity, and administrative simplicity carries through to the cost of the service. 5ACVO’s credentialing rates are fixed without hidden or confusing fees. These costs can be better for medical practice budgets without ongoing concern about new employee training or employee turnover.
Complex and careless credentialing can be costly.
Medical offices that do their primary source verification credentialing have to perform more work. It takes time and staff members to see the credentialing process to its end. Even if they complete every step flawlessly, they still do a lot of work that could be outsourced to a CVO like 5ACVO. When a provider needs to be credentialed again, the entire process must be repeated. Using 5ACVO to perform medical credentialing could free office staff from those tasks so they can focus on improving their organization in other ways, like generating more revenue or reassigning staff to areas where they are better suited.
There are numerous negative results of careless credentialing. Credentialing results can become disastrous if we make it overly complex.
Some results of careless, overly complex credentialing include:
- Medical staff membership and privileges are delayed.
- Current employment and contracts are adversely affected.
- Future employment harmed.
- NPDB reporting errors.
- Licensure delayed or restricted.
- Payor credentialing enrollment errors.
- The provider’s reputation and life can be tarnished.
Read more in 7 Results Of Careless Credentialing.
5ACVO’s Highly Effective Credentialing Team
5ACVO’s smarter credentialing can lighten a practice’s expenses and workload. Sometimes a person’s morale can improve when not faced with a barrage of duties. Their stress levels might also see a reduction. People might work better if they are not inundated with challenging assignments. They also might not make as many mistakes during their workday, especially if they do one of the 52 conventional credentialing steps.
5ACVO is dedicated to making medical credentialing better and easier for its members. This one purpose can result in a chain of improvements that affect levels of patient care, profit margins, amounts of work, and personal satisfaction.
Founded in 2003, 5ACVO has served 6,700+ providers, medical staff, facilities, hospitals, and physician practices throughout the United States. With 385+ years of industry knowledge, 5ACVO is the premier medical credentialing team. 63% of the company’s employees have 10+ years of industry experience.
5ACVO enjoys synergy with the other companies under the Fifth Avenue Healthcare Services banner. Primoris Credentialing Network is the largest independent physician association (IPA) in the Midwest and one of the only credentialing IPAs in the country. Fifth Avenue Agency uses the credentialing data and technology of the Fifth Avenue Healthcare Services group to expedite medical malpractice insurance shopping. This creates a competitive market that can result in lower rates. Their administrative simplicity helps make people’s lives better.
More information about 5ACVO
5ACVO is a NCQA Credentialing Accredited specializing in credentialing and primary source verification and is part of the Fifth Avenue Healthcare Services family. 5ACVO sister companies include Fifth Avenue Agency (MPLI and medical malpractice insurance specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
5ACVO originally published this article here. For more information on 5ACVO, please visit 5ACVO.com or Contact Us.