In what many call a shock verdict, Thapa v. St. Cloud Orthopedic Associates ended when a federal jury awarded the plaintiff a record $111 million in damages. This marks MN’s largest medical malpractice verdict in history.
St. Cloud Orthopedic Associates allegedly failed to diagnose and adequately treat Thapa after the plaintiff underwent leg surgery. Thapa developed acute compartment syndrome, which causes pressure in a grouping of muscles, nerves, and blood vessels. This pressure can result in muscle and nerve damage as well as pain. This condition usually occurs within hours of the inciting incident. The effectiveness of treatment heavily depends on how fast it is administered. Although treatable, this condition can be life-threatening, sometimes causing amputation, infection, renal failure, or death.
Thapa claims that the orthopedic practice’s providers did not promptly diagnose and treat this condition, which might have been a critical error. Regardless, the oversight is an expensive one.
Of the $111 million award:
- Approximately $500,000 is for past medical expenses.
- Roughly $800,000 is for future medical costs.
- $10 million is for past pain and suffering.
- $100 million is for future pain and suffering.
- No damages were awarded for lost earning capacity.
This verdict was made possible by a previous medical malpractice lawsuit, Popovich v. Allina Health. The MN Supreme Court ruled that a hospital can be held liable for its independent contractor’s negligence. This monumental decision reversed a long-standing rule that hospitals could only be held responsible for their employee’s actions.
Although some experts predict the verdict to be appealed or settled, the Thapa case could usher in sweeping changes to medical malpractice claims, raising insurance premiums. It could also cause hospitals and other medical organizations to reevaluate their relationships with independent contractors.
More Medical Malpractice Verdicts for the Record Books
This historical verdict comes on the heels of another record-setting trial. An Iowa jury awarded $97.4 million to the family of a child born with brain damage due to negligence. The Kromphardt family alleges that a cesarean section was required, but the physician continued with a vaginal birth. The child suffered from oxygen deprivation and a skull fracture when the physician allegedly disregarded protocol when she used a vacuum extractor to remove the baby.
That verdict was the largest of its kind in Iowa history. However, these two verdicts do not come close to the most significant medical malpractice award in the United States. A Maryland jury awarded Erica Byrom $229 million after her daughter suffered a brain injury during birth. The state cap lowered the total to $205 million. Physicians told Byrom that her baby was non-viable when it was not. The child suffered oxygen deprivation and will require care for the rest of her life.
Medical Malpractice Statistics
- Over the past 30 years, Minnesota has seen 19,043 medical malpractice lawsuits. The national average is approximately 47,000.
- The total payout over these 30 years is $1.2 billion+.
- The average payout is $64,910 against the national average of $101,716.
- The average award in Minnesota is $52,352.
- There were 812 lawsuits in 2019.
- The statute of limitations to file a medical malpractice lawsuit in Minnesota is four years.
Medical Malpractice Examples
Example 1: $4.2 Million Spine Injury
A patient underwent a cervical diskectomy and fusion. She received a spinal cord injury when the anesthesiologist applied traction to her cervical spine. The patient’s injury resulted in permanent quadriplegia. The woman received a settlement of $4,250,000.
Example 2: $2 Million Failure To Diagnose
A failure to diagnose a man’s heart problems resulted in emergency surgery led to a $2 million settlement. The man had received cardiac care from the same primary care physicians for nearly 30 years when in 2007, he suffered a massive aortic dissection. His physicians diagnosed him with a bicuspid aortic valve, which meant he would likely develop an aortic dissection. However, the man alleged that he was never referred to a cardiologist for proper treatment.
Example 3: $980,000 Kidney Stone Infection
A woman had kidney stone surgery, and her surgeon failed to diagnose and treat an infection that appeared. The infections spread to her fingers and toes, which had to be amputated. The woman received a $980,000 settlement.
The Most Common Reasons for Medical Malpractice Claims
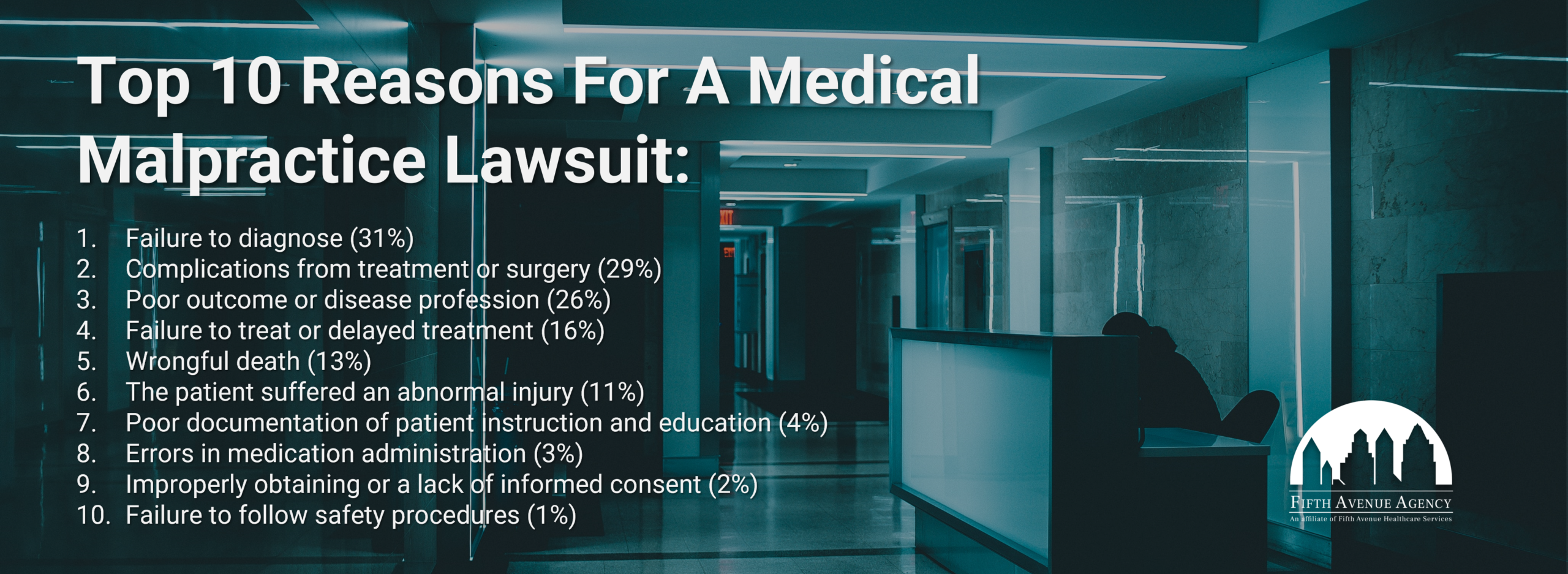
A recent Medscape study listed the top 10 reasons for medical malpractice lawsuits in 2021:
- Failure to diagnose
- Complications from treatment or surgery
- Poor outcome
- Failure to treat
- Wrongful death
- The patient suffered an abnormal injury
- Inadequate documentation of patient instruction and education
- Errors in medication administration
- Improperly obtaining or a lack of informed consent
- Failure to follow safety procedures
What is a Failure to Diagnose?
A failure to diagnose is an error that sees physicians not communicating conditions and treatments to their patients. Approximately 75% of injuries originating from diagnostic errors concern vascular events, infections, and different types of cancer. Nearly 12 million Americans experience diagnostic errors every year. Experts believe these mistakes are so common that everyone might fall victim to such an error at some point.
A Johns Hopkins University School of Medicine study concluded that 35+% of medical malpractice payments resulted from diagnostic errors.
What is a Failure to Treat?
A physician’s failure to treat a patient can worsen the patient’s condition, causing other problems that cause mental and physical pain. These occurrences commonly happen when patients are released too quickly and are not followed up on.
A 2021 survey found that 16% of malpractice lawsuits were filed due to physicians allegedly failing to treat their patients.
What Makes a Medical Malpractice Lawsuit Viable?
For a medical malpractice suit to be deemed viable, plaintiffs must have the ‘4 Ds’ of Medical Malpractice, duty, direct cause, dereliction, and damages.

The 4 D’s of medical malpractice include:
- Duty: A professional relationship between a physician and their patient must exist and be proven. It must be understood that physician will treat their patient to the best of their abilities and the standards of medicine.
- Direct cause: Plaintiffs must prove that their physician’s deviation from accepted standards of care caused their injuries. Examples include physicians misdiagnosing a patient, misreading test results, and recommending unnecessary or incorrect surgery.
- Dereliction: Plaintiffs must prove their physician caused harm in a way that a more effective doctor would not have.
- Damages: Only damages like physical pain, mental anguish, and lost earning capacity are eligible for compensation.
What Can Practices and Providers Do to Reduce Their Malpractice Risk?
The rise in costly malpractice verdicts can give even the most proficient healthcare provider pause. They can protect themselves by following the 4 C’s of Medical Malpractice Prevention and owning sufficient medical malpractice and medical professional liability insurance.
Practices Can Outsource Credentialing
Healthcare providers must be credentialed before they are allowed to treat patients. Occasionally, providers and practices perform the complicated process themselves. It involves gathering and assessing numerous informational items to verify a provider’s identity and experience.
Conventional credentialing consists of 52 action items, including:
- Assessing medical malpractice claims history.
- Authenticating medical school internship, residency, fellowship, and affiliations.
- Researching primary and out-of-state licenses for disciplinary actions.
- Obtaining a copy of the provider’s current certificate of insurance.
- Confirming any Medicare and Medicaid sanctions and exclusions.
- Performing an extensive 10-year criminal background check.
- Running a National Practitioner Data Bank query.
If in-office staff perform credentialing, they risk making mistakes that can pass an unqualified provider through or stop a perfectly-capable one from practicing medicine. In addition, credentialing can take a lot of time. Staff might not have time to perform their other duties.
Outsourcing the process to a credentials verification organization like 5ACVO can reduce errors and save office staff time and money. The faster providers can be credentialed, the sooner they can bill for their services.
Practices Can Better Inform Patients
Practices can determine if their current and future independent contractors and credentialed medical staff members must increase their insurance coverage. They can also make clear delineations between contractors and employees. Uniforms, badges, and signs can be used to inform patients that contractors may treat them.
Practices Can Focus On The 4 Cs of Medical Malpractice Prevention
Healthcare providers who practice the ‘4 Cs’ of medical malpractice (compassion, communication, competence, and charting) can reduce their chances of being named in a medical malpractice lawsuit.
The 4 C’s of medical malpractice include:
- Compassion: Care and sympathy can go a long way in protecting physicians. Compassionate physicians are typically honest and openly communicate with their patients.
- Communication: Proper communication, like listening and clearly explaining diagnoses and treatment plans, can reinforce the bond between physicians and their patients.
- Competence: Simply put, physicians must know what they are doing. They have to follow accepted standards of care set forth by the medical industry. They should also keep up with contemporary trends in healthcare.
- Charting: Thoroughly recording patient symptoms charting can reduce diagnostic and treatment errors.
Providers Can Be Adequately Insured
Providers should review insurance policies to protect them from costly claims and litigation. If they find they are not, they can seek assistance from insurance experts who can get them the protection they need. Fifth Avenue Agency can analyze medical malpractice needs and communicate a custom solution. Once a provider accepts the proposal, we can quickly and efficiently implement the plan. We want to help providers reduce their costs and help mitigate their medical liability.

Suppose providers choose to shop for medical malpractice insurance themselves. In that case, they should research the following three financial strength factors to consider in selecting a medical malpractice carrier along with the following essential items to make the best decision:
- The percentage of the carrier’s claims that are closed without payment. A study of 7 states (Florida, Illinois, Maine, Massachusetts, Missouri, Nevada, and Texas) found that most medical malpractice claims were closed without payment. How often a carrier can prevent lawsuits from going to court shows how effectively they protect their insured’s best interests.
- The carrier’s trial win percentage. Providers should seek a carrier that can go to court and win their cases. Some studies find that the average carrier wins 50% of trials when faced with compelling evidence of medical negligence. They win approximately 90% of cases featuring weak evidence.
- The carrier’s A.M. Best rating. The A.M. Best Company is one of the most trusted industry analysts with insurance carrier ratings. An A.M. Best rating estimates a carrier’s ability to pay its debts. A financially healthy carrier can pay out if it loses a medical malpractice suit.
- Coverage cost. Medical malpractice insurance costs can be expensive depending on the specialty, the state where the physician practices, and the required coverage. Higher-risk specialties yield more significant rates than family practice providers. States with many medical malpractice claims might require insureds to pay more.
- The medical malpractice policy limit. How much a carrier will pay out should be vital in decision-making. The policy limit is the coverage amount for a given policy period. It is usually shown as “per claim” and “aggregate.” The per-claim amount is what the carrier will pay for each claim. The aggregate amount is what the carrier will pay during the policy period. A carrier can pay for multiple claims if they fall within the aggregate amount.
Conclusion
Medical malpractice can be a costly nightmare for healthcare providers and patients. Providers who cannot perform their medical duties can injure those who trust them with their well-being. Providers who go beyond can also fall prey to meritless claims. Fifth Avenue Agency and its sister companies can help protect providers and patients from malpractice.
Providers can trust the Fifth Avenue family to properly credential them so they can continue their medical careers untethered by suspicion. They can practice medicine while sufficiently covered by insurance that aligns with their needs. Taking the proper approach can prevent a $111 million verdict from ruining a provider and their practice.
More information about Fifth Avenue Agency
Fifth Avenue Agency specializes in MPLI and medical malpractice insurance, serving 1000s of providers nationwide. Fifth Avenue Agency is part of the Fifth Avenue Healthcare Services family. Sister companies include 5ACVO (credentialing and primary source verification specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
For more information on Fifth Avenue Agency, please visit FifthAvenueAgency.com or Contact Us.