Medical providers, we know how it goes: you’ve got a mountain of tasks, with credentialing being one of the first steps to creating a new working relationship that brings a slew of things that need to be done. This can take a toll on providers and subtract valuable resources from patient care.
Primoris Credentialing Network, one of Fifth Avenue Healthcare Services’ sister companies, can help smooth the credentialing process by allowing you to use delegated provider enrollment.
What is Delegated Provider Enrollment?
Got a lot of credentialing and enrollment paperwork stacked on your desk and wished someone else could take some of the load? Delegated health plan enrollment may be a good solution for you.
NCQA states “delegation occurs when an organization gives another entity the authority to carry out a function that it would otherwise perform.”
According to the NPDB, “Delegated credentialing occurs when a health care entity gives another health care entity the authority to credential its health care practitioners.”
Delegation from health plans can be hard to achieve. Not only does it take a high volume of providers, but it also takes years of proven quality, detailed policies and procedures, and the ability to pass stringent audits every year. But the power to improve the enrollment process through delegation is significant. In this case, delegated provider enrollment is accomplished when a payer delegates the credentialing and health plan enrollment to Primoris Credentialing Network, an IPA. Primoris has agreements in place and positive working relationships currently with some 54+ health plans and networks options.
Through delegated provider enrollment, Primoris completes the credentialing and enrollment of its member providers through a single process applied to multiple health plans, submitting and following up with the health plan(s) until the desired enrollment is complete. This usually results in more favorable effective dates, weeks, or months shaved off of the timeframe and, ultimately, better patient care and increased billing.
According to NAMSS, there are numerous reasons to delegate, including these seven (7) positive outcomes for delegating:
- Reducing turnaround time for network participation
- Helps manage a significant volume of providers
- Reduces resources (staff, budgets, time)
- Accommodates network growth
- Reduces turnaround time for network participation
- Timelier reimbursement from payers
- Increases practitioner satisfaction
Using delegated provider enrollment allows us to add a provider to multiple health plans at once, which is much more quickly than the typical enrollment method. Without delegation, the traditional method is to send an application to each health plan individually. With delegation, sending numerous applications is unnecessary, but you can work with Primoris through delegation where we will enroll a provider in multiple health plans through our delegation process. This benefit lets providers begin billing and seeing patients much sooner than they otherwise would.
Track Record Of Success
Primoris has worked with 1000s of providers over the past decade, becoming the largest credentialing IPA in the Midwest. Primoris Credentialing Network has 54+ health plans and network options, many available with delegated enrollment. By partnering with Primoris, you can rest assured knowing that our team of experts with 385+ years of combined experience will go to work for you and your team.
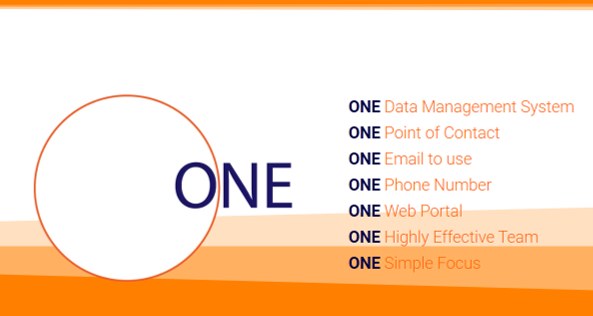
You can become the CEO of Credentialing and Provider Enrollment, communicating with your Primoris team through ONE point of contact using ONE email, ONE phone number, and ONE web portal that will give you 24×7 access to monitor our credentialing and enrollment progress.
Additionally, once your provider(s) are enrolled, you can access the Primoris Credentialing Web Portal anytime to view, print, import/export all your credentialing and enrollment data. Be confident knowing exactly where things stand for any specific number of your providers in the credentialing and enrollment process using the credentialing web portal.
Non-Delegated Enrollment
By allowing providers to submit everything under a single application (delegation), the credentialing process can be completed faster than ever before; however, there may be circumstances or a plan in which we do not have a delegated agreement that makes it best to use a non-delegation model which we will fully administrate, from obtaining the first signature to notifying you of complete enrollment.
Primoris Quick History
Since our launch over a decade ago, Primoris Credentialing Network has become the largest credentialing and enrollment IPA in the Midwest. Now, medical providers can choose from 54+ health plans and network options based on the needs of their patients.
The Primoris team has 385+ years of combined industry experience, and 63% of this stellar team has more than ten years of experience each. All of us on the Primoris team continually strive to provide the highest quality services to all our providers; whether they use our delegated or non-delegated health plan enrollment services, Primoris has your back.
With a team of experts on your side and the most up-to-date technology underpinning our provider web portal, providers can easily knock out credentialing enrollment. Another benefit to you is storing all your information in a single, secure database that you can easily access anytime from anywhere.
More information about Primoris Credentialing Network
Primoris Credentialing Network is a NCQA Credentialing Accredited specializing in credentialing and provider enrollment with 54+ health plan and network provider enrollment options. Primoris is a family member of Fifth Avenue Healthcare Services. Sister companies include 5ACVO (credentialing and primary source verification specialists) and Fifth Avenue Agency (MPLI and medical malpractice specialists).
Primoris Credentialing Network originally published this article here. For more information on Primoris Credentialing Network, please visit PrimorisCredentialingNetwork.com or Contact Us.